Pharmacokinetics
Scroll down to learn about pharmacokinetics.
In this section you will learn about pharmacokinetics. You will encounter these concepts on school and national exams and on a daily basis at work, although you may not use those exact terms. Patients will ask questions about how their medications work, and the knowledgeable medical professional will be able to answer their questions with confidence.
Click through the toggles to learn about pharmacokinetics or skip down the page to play the games.
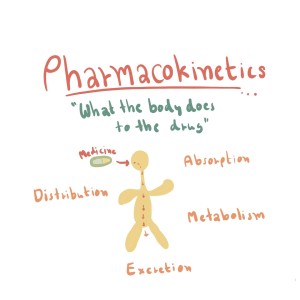
- Absorption: This process refers to how a drug moves from its site of administration into the bloodstream.
- Distribution: After a drug enters the bloodstream, it distributes throughout the body and reaches the target tissues or organs.
- Metabolism: Most drugs undergo chemical changes in the body, primarily in the liver, through various enzymatic reactions. These changes, known as biotransformations, can lead to the formation of active or inactive metabolites.
- Excretion: The final pharmacokinetic process is the elimination of the drug and its metabolites from the body, primarily through renal (kidney) or hepatic (liver) routes.
Pharmacokinetics may at first sound intimidating, but let's bring it back down to Earth. Picture it as a fascinating journey of a medication inside our body, similar to the dramatic arc of a novel with four main stages: absorption, distribution, metabolism, and excretion. Let's call these stages ADME for short, the ABCs of pharmacokinetics.
1. Absorption: Tickets, Please!
Imagine you've just taken a pill for a pesky headache. This pill, let's call it our protagonist, starts its journey in your body via absorption. Absorption is all about how the drug moves from the outside world into your bloodstream. Think of it as the drug getting its ticket punched for the train ride at the station. Depending on the route of administration, this station could be your stomach, your intestines, or even your skin.
...........The full text is available to members.
Absorption is the first step in the pharmacokinetic process and refers to the passage of a drug from its site of administration into the systemic circulation (bloodstream). It is a crucial step that determines the onset, intensity, and duration of a drug's action in the body.
- The rate of absorption determines how soon the drug will take affect.
- The amount of absorption determines the intensity of the drug's effect.
...........The full text is available to members.
Distribution is the second step in the pharmacokinetic process, referring to the transport of a drug from the bloodstream to various tissues and organs throughout the body. Once a drug is absorbed into the systemic circulation, it can either remain in the bloodstream or distribute to the target and non-target tissues. The extent and rate of distribution are crucial in determining the drug's therapeutic effects and potential side effects. Several factors can influence drug distribution:
...........The full text is available to members.
Metabolism is the third step in the pharmacokinetic process, which involves the biotransformation of a drug into different chemical compounds, known as metabolites. The primary goal of drug metabolism is to convert lipophilic (fat-soluble) drugs into more polar (water-soluble) metabolites, making them easier to excrete from the body. Metabolism can also result in the activation or inactivation of a drug, impacting its therapeutic effects and potential side effects. The liver is the primary organ responsible for drug metabolism, although other tissues, such as the gastrointestinal tract, kidneys, and lungs, may also contribute.
...........The full text is available to members.
Excretion is the fourth and final step in the pharmacokinetic process, which involves the elimination of drugs and their metabolites from the body. The primary goal of excretion is to remove these substances to prevent their accumulation and maintain a balance within the body. Efficient excretion is essential for terminating a drug's action and preventing potential toxicity. There are several routes and mechanisms of excretion, with the kidneys and liver being the most important organs involved.
...........The full text is available to members.
Terms to Know - Pharmacokinetics
Pharmacokinetics also refers to the movement of a drug throughout the body.
Each phase of pharmacokinetics - absorption, distribution, metabolism, and excretion - involve drug movement through membranes. Drugs pass through membranes in a variety of ways but three are most important - Direct penetration, facilitated diffusion, and active transport.
- Direct penetration is the process by which drugs cross biological membranes, such as the cell membrane's phospholipid bilayer, by passive diffusion without the need for membrane transporters, channels, or the expenditure of energy. This is the most common method of drug transport as most drugs are too large to fit through channels and pores and most lack a transport system.
Drugs that are lipid soluble are absorbed more rapidly because they can readily cross cell membranes.
Cell membranes are composed of bilayers of lipids (fats) and phosphate "tails." A common rule of chemistry is that "like dissolves like." Because cell membranes are composed of lipids, a drug must be lipid soluble (lipophilic - "lipid loving") to directly pass through a cell membrane. Some drugs are not lipophilic, rather they are hydrophilic (water loving) and cannot pass through cell membranes via direct penetration. Think about mixing water and oil. You can shake ajar of the two, but they will never dissolve into each other. They separate and settle into layers.
-
Facilitated Diffusion - This mechanism involves the passive movement of drug molecules across membranes with the help of specific carrier proteins. Facilitated diffusion does not require energy expenditure but is limited by the availability of carrier proteins and can become saturated at high drug concentrations.
-
Active Transport - In this process, drug molecules are transported across membranes against their concentration gradient with the help of carrier proteins and energy derived from ATP (adenosine triphosphate). This mechanism allows the absorption of drugs that are not easily absorbed by passive diffusion or are too large to pass through membrane pores.
Minimum Effective Concentration (MEC) refers to the lowest concentration of a drug in the bloodstream that is required to produce a desired therapeutic effect.
If the drug concentration falls below the MEC, the therapeutic effect may be insufficient or lost, leading to suboptimal treatment outcomes.
Toxic concentration refers to the level of a drug or substance in the bloodstream at which it causes harmful or adverse effects on the body. When the concentration of a drug exceeds the maximum safe concentration (MSC) and enters the toxic range, it can lead to undesirable side effects, organ damage, or even life-threatening situations.

A higher therapeutic index indicates a wider margin of safety, as there is a greater separation between the effective dose and the toxic dose. In other words, a drug with a high TI is considered safer because there is a lower risk of toxic effects at therapeutic doses.
Conversely, a drug with a low therapeutic index has a narrow margin of safety, meaning that even small changes in the dosing regimen or individual patient factors could lead to toxic effects.
Trough level - Also known as the minimum concentration, refers to the lowest concentration of a drug in the bloodstream, typically measured just before the administration of the next dose.
It is commonly used in therapeutic drug monitoring to ensure that drug concentrations remain within the therapeutic range, which is the range of drug concentrations associated with optimal efficacy and minimal side effects.
Monitoring trough levels is particularly important for drugs with a narrow therapeutic index, where small changes in drug concentrations can lead to significant differences in therapeutic effects or toxicity.
Eexamples of such drugs include
- vancomycin
- lithium
- digoxin
- warfarin
The half-life of a drug is a pharmacokinetic parameter that represents the time it takes for the concentration of the drug in the body to decrease by half. It helps healthcare professionals determine the appropriate dosing frequency and duration of treatment.
Half-life is influenced by two main processes: absorption and elimination. Absorption refers to how a drug enters the bloodstream, while elimination refers to the removal of the drug from the body, either through metabolism or excretion.
Several factors can affect a drug's half-life, including:
-
Drug formulation: The formulation of a drug, such as immediate-release or extended-release tablets, can impact its absorption rate and thus its half-life.
-
Route of administration: The way a drug is administered (e.g., oral, intravenous, intramuscular) can affect its absorption and elimination, impacting the half-life.
-
Metabolism: The rate at which a drug is metabolized in the body can influence its half-life. This rate can vary among individuals due to factors such as genetics, age, and co-existing medical conditions.
-
Elimination: The efficiency of the body's organs, such as the liver and kidneys, in eliminating a drug can affect its half-life. Factors like renal or hepatic impairment can significantly extend drug half-life.
Drugs with a short half-life may need to be administered more frequently to maintain their therapeutic effect, while those with a long half-life may require less frequent dosing.
Plateau drug levels, also known as steady-state concentrations, refer to the point at which the rate of drug administration (input) is equal to the rate of drug elimination (output) in the body.
At this stage, the drug concentration in the bloodstream remains relatively constant, fluctuating within a narrow range around an average value. Achieving plateau drug levels is crucial for maintaining consistent therapeutic effects during the course of treatment.
After repeated and regular administration of a drug, it typically takes about 4-5 half-lives for the drug to reach steady-state concentrations. The half-life of a drug is the time it takes for the drug's concentration in the body to decrease by 50%. For drugs with short half-lives, plateau levels are reached relatively quickly, while drugs with long half-lives may take days or even weeks to reach steady-state concentrations.
In some cases, therapeutic drug monitoring may be employed to measure drug concentrations in the patient's blood, allowing for adjustments in dosing to maintain plateau levels within the desired therapeutic range.
A loading dose is an initial, higher dose of a drug administered at the beginning of treatment to rapidly achieve the desired therapeutic concentration in the bloodstream.
This practice is particularly useful for drugs with long half-lives, as it can take a significant amount of time to reach steady-state concentrations with regular dosing alone. The loading dose helps to quickly establish an effective drug concentration, allowing the desired therapeutic effect to be achieved sooner.
After administering the loading dose, maintenance doses are given at regular intervals to maintain the therapeutic drug concentrations within the desired range.
Course and Games to Test Your Knowledge
Click on the corresponding image below to test your knowledge of pharmacokinetics. The mini course allows you to choose between flashcards, a randomized quiz, as well as line-'em-up and drag-and-drop interactions. The other options are games with rationales.
|
Pharmacokinetics Mini Course The course is available to members.
|
|
|
Pharmacokinetics 1 Printouts available to members |
Pharmacokinetics 2 Available to members |